Best Diet for PCOS: Low-Carb and Alternatives
The best PCOS diets, from low-carb to low-GI, Mediterranean, and DASH, with evidence on insulin, weight, and cycles.
Clear, evidence-based dietary patterns to manage insulin resistance, weight, and symptoms in PCOS.
Key takeaways
- Low-carb works for many with PCOS, but it is not the only effective option.
- Low-GI, Mediterranean-style, and DASH patterns also improve weight, insulin markers, and cycles.
- Sustainable calorie deficit and consistent meals often matter more than one “perfect” diet.
This article is educational. Discuss any diet changes with your clinician, especially if you use glucose-lowering meds or are trying to conceive.
Low-carb for PCOS: what the evidence says
Low-carb approaches target insulin resistance, a core PCOS driver. Clinical reports and small trials show weight loss, improved insulin, and more regular cycles with carbohydrate restriction. Ketogenic or very-low-carb plans can accelerate early results, but data sets are small and adherence varies. Personalization and medical oversight are essential, particularly for those on metformin or with lipid issues.
Ketogenic diet (very-low-carb)
Short trials of keto-style plans in overweight women with PCOS reported reductions in weight and androgens and menstrual improvements over 8–12 weeks. Evidence quality is limited and sample sizes are small, so long-term superiority over moderate low-carb is unproven. Typical study targets: ~5–10% energy from carbs (<30 g/day).
Moderate low-carb
Moderate low-carb (for example, 25–40% carbs) often balances satiety, fiber, and adherence. It can reduce glycemic load without eliminating whole food groups.
Low-carb swaps that preserve fiber
- Replace white rice with quinoa or cauliflower rice.
- Swap sugary cereal for Greek yogurt + chia + berries.
- Use legumes and tofu in place of processed meats.
Low-Glycemic Index (GI) eating
Low-GI plans prioritize carb quality over strict carb counts. Randomized trials show low-GI diets reduce body weight and central adiposity and can increase ovulatory cycles in anovulatory PCOS. Many find this more sustainable than very-low-carb because whole-grain breads, oats, legumes, and fruit remain in rotation.
What improves
Typical gains include lower fasting insulin, improved HOMA-IR, and reduced cravings due to more stable glucose. Takeaway: ideal if you want flexibility with carbs while controlling spikes.
Study-style macros
Common research patterns: ~20% protein, ~30% fat, ~50% low/medium-GI carbohydrates with a daily 300–500 kcal deficit.
Example low-GI day
| Meal | Option | Why it helps |
|---|---|---|
| Breakfast | Oats + berries + nuts | Fiber slows glucose |
| Lunch | Lentil salad + olive oil | Protein + MUFAs |
| Snack | Greek yogurt + chia | Protein + satiety |
| Dinner | Salmon, broccoli, barley | Low-GI carbs, omega-3s |
When in doubt, pair carbs with protein + fat to blunt glycemic response.
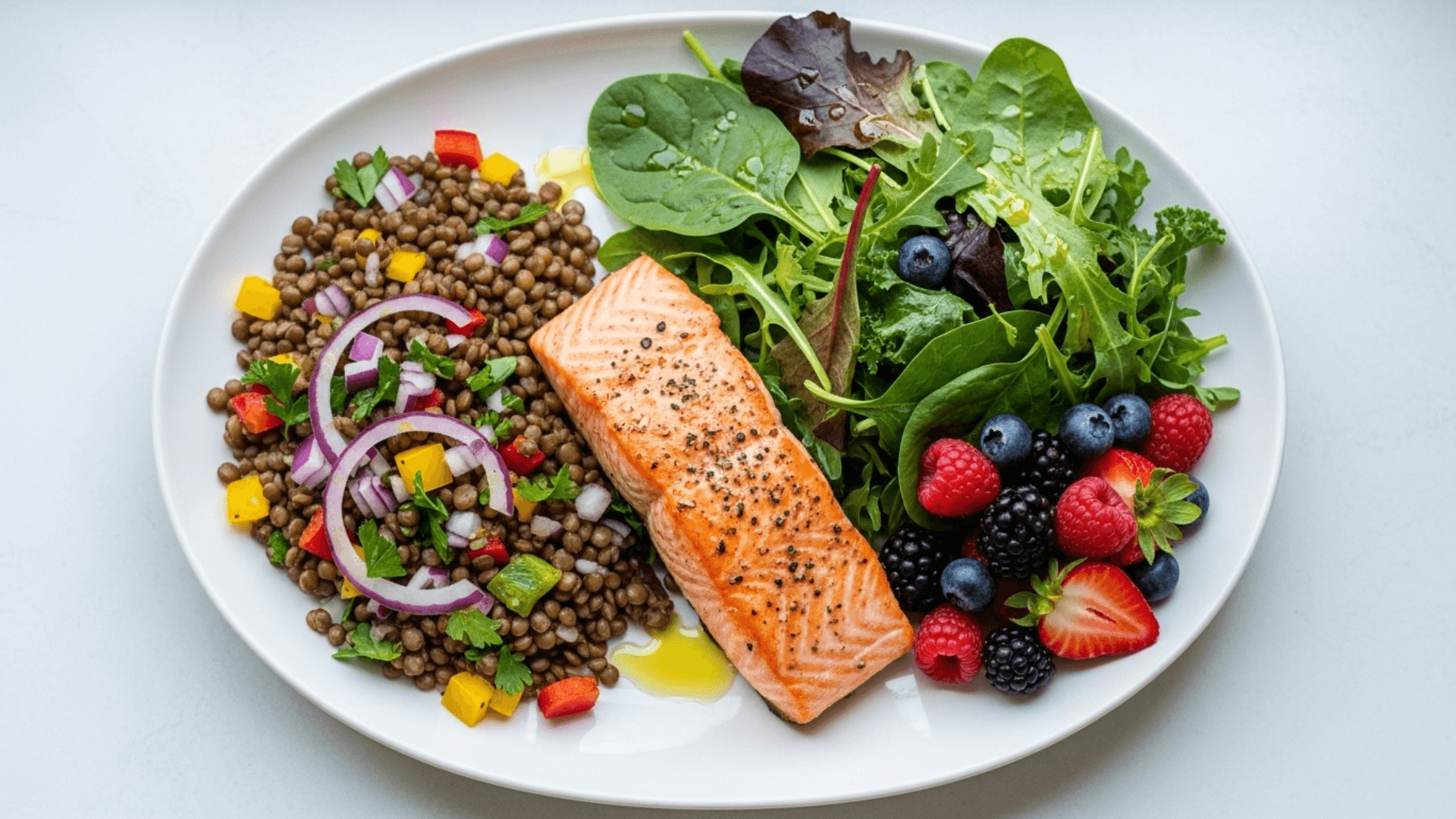
Mediterranean-style patterns
Dietitians often recommend a Mediterranean pattern for PCOS: vegetables, fruit, legumes, whole grains, fish, nuts, and olive oil. Observational and interventional studies associate higher Med-diet adherence with better metabolic markers; a Mediterranean + low-carb model restored cycles and improved endocrine profiles more than a low-fat plan in overweight PCOS populations.
Who it fits
You want variety, cardiovascular protection, and family-friendly meals. The emphasis on unsaturated fats and minimally processed foods also aligns with anti-inflammatory goals. Takeaway: strong all-round choice, easy to sustain.
Med-style priorities for PCOS
- Extra-virgin olive oil over butter.
- Fish 2–3×/week; legumes several times weekly.
- Whole grains in measured portions with meals.
- Vegetables and fruit at most meals.
DASH and anti-inflammatory options
Randomized trials of DASH in PCOS show benefits for BMI, insulin, hs-CRP, and lipid profiles over 8–12 weeks when energy-restricted. DASH emphasizes vegetables, fruit, whole grains, low-fat dairy, lean proteins, and low saturated fat. Anti-inflammatory patterns similarly prioritize whole foods and healthy fats while minimizing refined sugars and processed meats.
Practical fit
DASH suits those with hypertension risk or who prefer structured food groups without very low carbs.
DASH vs Mediterranean (at a glance)
| Feature | DASH | Mediterranean |
|---|---|---|
| Primary aim | BP and metabolic health | Cardiometabolic and longevity |
| Dairy | Low-fat emphasized | Optional, usually low-to-moderate |
| Fats | Lower sat fat overall | Higher MUFAs (olive oil) |
| Evidence in PCOS | RCTs show improved insulin/hs-CRP | Observational + interventional trends |
Many “anti-inflammatory” lists mirror Med/DASH foods; focus on patterns, not superfoods.
Calories, timing, and sustainability
Weight loss of ~5–10% in those with overweight can improve cycles and ovulation rates in PCOS. Lifestyle RCTs show preconception weight loss enhances ovulation and live births compared with immediate fertility medications. Set a realistic energy deficit and monitor progress with your clinician.
Meal timing
Consistent, balanced meals every 3–4 hours can help avoid large glucose swings and curb overeating. Intermittent fasting is popular, but clinicians caution that blood sugar stability is a priority in PCOS; more research is needed before broad use.
Track protein at ~20–30 g per meal and fill half your plate with non-starchy vegetables.
Building your PCOS plate
Plate method
- ½ plate: non-starchy vegetables.
- ¼ plate: protein (fish, poultry, tofu, eggs, legumes).
- ¼ plate: low-GI carbs (oats, barley, quinoa, beans).
- Add: olive oil, nuts, seeds; water, tea, or coffee unsweetened.
Checklist (weekly)
- Fish 2–3×; legumes ≥3×; nuts/seeds most days.
- Whole grains in measured servings; limit refined flour and sugary drinks.
- Prepare snacks that pair carb + protein.
If you are lean with PCOS, do not chase weight loss. Focus on glycemic quality, protein, and adequate total energy.
References
- DASH RCTs: PMID 24956415, 25194966, 28316072.
- Low-GI and ovulation: PMID 29734548; review PMC 8600081.
- Mediterranean + low-carb: PMID 35445067; narrative reviews 39558903.
- Keto in PCOS: PMID 32103756, 33462940; meta-analysis PMC 10484165.
- Clinical overviews: Johns Hopkins PCOS Diet; Verywell Health PCOS Diet; Cleveland Clinic ConsultQD.
Frequently Asked Questions
Both can work. Low-GI has RCT support for weight and ovulation, while low-carb reduces insulin load and may speed initial loss. Choose the pattern you can sustain.
Short-term studies show benefits in weight and hormones, but evidence is limited and adherence is hard. Use clinically supervised plans and reintroduce whole-food carbs as soon as feasible.
About 5–10% often improves cycles and ovulation; lifestyle RCTs show better ovulation and live birth outcomes before fertility treatment.
Not first-line for most with PCOS. Stable blood sugar and consistent meals are often preferable; more research is needed.
Avoid aggressive deficits. Use Mediterranean or low-GI patterns, prioritize protein and fiber, and ensure enough calories to maintain cycles.